Pancreas Anatomy, Function & Disease: All you need to know
The pancreas is a digestive and endocrine system organ found in all vertebrates, including humans. Situated in the abdominal cavity, it performs the function of a gland in humans and other primates.
The pancreas is a heterocrine gland, meaning that it plays the role of both an endocrine and exocrine gland in the digestive system. The exocrine portion of the pancreas accounts for 99 percent of its function, with the remaining 1 percent being endocrine.
Its primary role as an endocrine gland is to control blood sugar levels, and it does so by producing substances called hormones such as insulin, glucagon, pancreatic polypeptide and somatostatin.
It has an important role to play in the digestive system. It secretes pancreatic juice through its duct, directly into the duodenum. Bicarbonate is included in this juice, which aids in the neutralization of acid that enters the duodenum from the stomach.
The pancreas is an important organ in the treatment of diabetes mellitus and its involvement in controlling blood sugar levels.
It also neutralizes the digestive enzymes, which help break down the carbohydrates, proteins, and lipids present in the food we eat.
There are certain diseases related to the pancreas. Pancreatitis is an inflammation of the pancreas that may be caused by a variety of factors, including persistent alcohol use and stones.
Pancreatic cancer may develop as a result of chronic pancreatitis or for other causes, and it has a very bad outlook since it is frequently discovered after it has spread to other parts of the body. It can be fatal if left untreated.
Location and Anatomy:
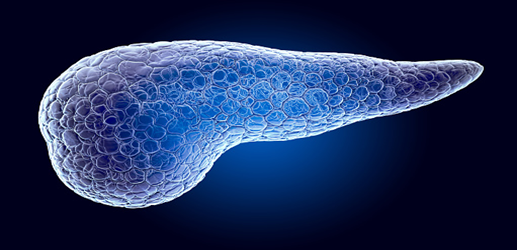
The pancreas is situated below the stomach in the upper left abdomen. Several different organs encircle the spleen, including the small intestine, spleen and liver. When fully expanded, it looks like a flattened pear or fish with the fins stretched horizontally over the abdominal region.
The widest portion of the pancreas, known as the head of the pancreas, is located towards the middle of the belly. The neck or body of the pancreas refers to the core portion of the organ. Lastly, the narrow end is referred to as the tail, and it continues to the left side of the body.

The pancreas is surrounded by many main blood arteries, including the superior mesenteric artery, celiac axis, superior mesenteric vein, and portal vein. All of these vessels are responsible for the provision of blood to the pancreas and other abdominal organs, including the liver.
Exocrine tissue, which accounts for nearly all of the pancreas (95 percent), is responsible for the production of pancreatic enzymes, which are necessary for digesting. The islets of Langerhans, which make up the remainder of the tissue, are endocrine cells.
These groupings of cells, which have the appearance of grapes, generate hormones that control blood glucose levels as well as pancreatic secretions.
Functions:
In order to digest the meals we consume, a healthy pancreas must generate the appropriate molecules in the proper amount at specific times. That's precisely how the pancreas functions; it releases enzymes and juices exactly when the body needs them.
Furthermore, the pancreas's function may be split into two categories: exocrine and endocrine.
Exocrine functions:
Exocrine glands in the pancreas are responsible for the production of enzymes that are essential for digestion.
These enzymes include trypsin and chymotrypsin, which aid in the digestion of proteins. Apart from it, amylase and lipase are likewise secreted, which help to digest carbohydrates and fats, respectively.
When food passes through the stomach, certain pancreatic fluids are discharged. After passing through the stomach, the pancreatic duct meets the common bile duct to create the ampulla of Vater. This landmark is situated near the beginning of the small intestine, the duodenum.

Endocrine functions:
The endocrine portion of the pancreas is made up of islet cells (islets of Langerhans), which are responsible for the production and release of essential hormones into the circulation.
Insulin, which works to decrease blood sugar levels, and glucagon, which functions to increase blood sugar levels, are two of the most important pancreatic hormones.
Whenever you eat a meal, insulin is produced. This would convert glucose into glycogen for storage, thereby decreasing blood sugar levels. Glucose is stored for future use in the liver, muscles and adipose tissues.
Whereas, when you are hungry or need glucose to combat any flight, fight or fright situation, glycogen would be converted into glucose by an enzyme called glucagon. This would raise your blood sugar levels and would give you the energy you need to function efficiently.
Blood glucose levels must be maintained in a healthy range for important organs such as the heart, liver, and lungs to operate properly.
Diseases of the Pancreas:
Pancreatitis:
Pancreatitis refers to a condition in which the pancreas gets inflamed. It is most often linked with repeated gallstones or persistent alcohol consumption.
Other reasons for pancreatitis are traumatic injury, impairment after an ERCP (a diagnostic procedure), certain medicines, diseases such as mumps, and very elevated blood cholesterol concentrations.
Pancreatitis causes severe abdominal pain that extends to the back and may be accompanied by nausea or vomiting. Acute pancreatitis is likewise linked with nausea and vomiting.
In extreme situations of pancreatitis, there may be bleeding or rupture of the pancreas, which may result in shock, severe distress or a systemic inflammatory syndrome. Other symptoms include discolouration of the flanks or the area around the belly button, among others.
These life-threatening problems are often treated in an intensive care unit (ICU).
If pancreatitis lasts for a longer length of time, it turns into chronic pancreatitis. The most frequent cause for this particular disease is chronic alcohol intake. Other reasons include repeated acute episodes of pancreatitis and cystic fibrosis, among others.
Cancer of the Pancreas:
Pancreatic malignancies, especially the most prevalent form, pancreatic adenocarcinoma, are very resistant to medical treatment. Moreover, they are often discovered at a stage when surgery, the only therapeutic therapy, is no longer an option.

Pancreatic cancer is very uncommon in individuals under the age of 40, with the typical diagnosis occurring at the age of 71. The following risk factors are associated with pancreatitis: chronic pancreatitis, advanced age, tobacco use, obesity, hypertension, and some uncommon genetic disorders.
Cancer of the exocrine digestive portion of the pancreas is the most prevalent kind of pancreatic cancer and is also known as pancreatic adenocarcinoma (also known as pancreatic cancer).
The majority of pancreatic cancers arise at the head of the pancreas. Indications of cancer usually appear later in the phase of the illness, when it develops signs such as stomach discomfort, loss of weight, or discolouration of the skin.
Jaundice likewise develops when the malignancy prevents the flow of bile from leaving the body. Headache, nausea, pancreatitis, hyperglycemia, and recurrent venous thrombosis are some of the less frequent symptoms of this condition.
Pancreatic cancer is often detected via medical imaging, such as an ultrasound or a CT scan with image enhancement, among other methods. A biopsy accompanied by ERCP or ultrasonography may likewise be performed depending on the disease condition.
Pancreatic cancer may manifest itself in a variety of ways, affecting both the endocrine and exocrine tissues. There are many different kinds of pancreatic endocrine tumours. However, they are all uncommon, and their prognoses are very variable.
Type 1 Diabetes Mellitus:
Diabetes mellitus type 1 is a chronic autoimmune illness in which the immune system attacks the insulin-secreting beta cells of the pancreas, resulting in insulin production being reduced or stopped. Insulin is required to stabilize blood sugar levels below optimum limits, and a shortage of insulin may result in elevated blood sugar levels.
If diabetes is left untreated for a long period, it may lead to consequences such as exacerbated vascular disease, diabetic retinopathy, renal disease, and neuropathy.
Likewise, it is possible to develop diabetic ketoacidosis if there is insufficient insulin to allow glucose to be used inside cells. Diabetic ketoacidosis is an emergency health condition and necessities immediate medical intervention.
Even though type 1 diabetes may develop at any age, it is most commonly recognized before the age of 40. Insulin injections are essential for individuals who have type 1 diabetes to stay alive and maintain their health.
Diabetes Mellitus type 2:
Diabetes mellitus type 2 is by far the most prevalent kind of diabetes. Type 1 diabetes is comparatively rare.
It is usually a mixture of insulin insensitivity and decreased insulin secretion that results in elevated blood sugar levels in this type of diabetes. Both environmental and genetic factors have a role in the progression of the disease.
Type 2 diabetes is managed via a mixture of lifestyle modifications, medicines (if necessary), and, in some cases, insulin injections (if necessary).
How Can You Keep Your Pancreas Healthy?
Maintaining a nutritious diet and refraining from smoking and excessive drinking can assist in maintaining the pancreas in good condition.
The National Pancreatic Foundation recommends that you do the following:
- Not over 20 grammes of fat per day in one's diet
- Refraining from consuming alcoholic beverages
- Drinking lots of water to stay hydrated is essential.
Following a fasting diet may cause the pancreas to rejuvenate, which may be beneficial for individuals with diabetes, per the findings of animal research released in February 2017.
A fast would include eating much fewer calories than average over several days.
For individuals who are suffering a flare-up of pancreatic discomfort, the National Pancreatic Foundation recommends an approach that is similar to this. A clear liquid diet consisting of grape juice, broth, and cranberry juice should be followed for one to two days, according to the experts
A fast will not be able to supply all of the nutrients required for good health. Therefore, following a fast, individuals should make sure they consume healthy meals to replenish the nutrients they have lost.



